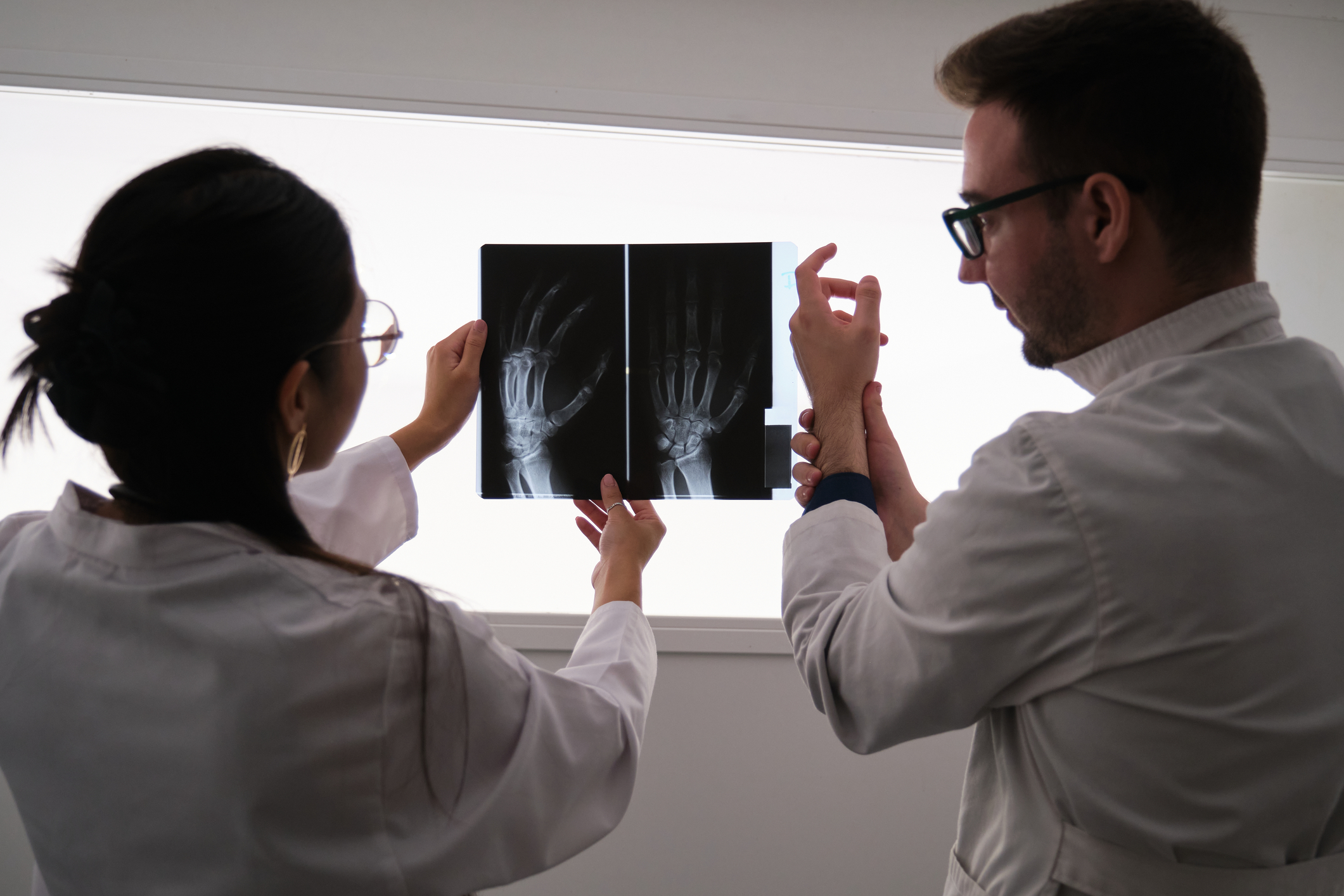
Your Complete Guide to Psoriatic Arthritis: From Symptoms to Solutions
Psoriatic arthritis (PsA) is a chronic autoimmune disease that not only affects the joints but also involves systemic inflammation impacting various organs. It merges symptoms of psoriasis—a skin condition characterized by red, scaly patches—with those of arthritis, including joint pain, swelling, and stiffness. This complex disease can significantly affect quality of life, and understanding its nuances can aid in better management and treatment.
Pathophysiology and Causes of Psoriatic Arthritis

Psoriatic arthritis is thought to arise from a combination of genetic predisposition, immune system dysfunction, and environmental triggers. Key factors include:
- Genetics: Over 40% of individuals with PsA have a family history of psoriasis or arthritis. Specific genetic markers, such as HLA-B27 and other HLA alleles, have been associated with increased risk, suggesting a strong genetic component.
- Immune System Dysregulation: PsA is characterized by the activation of T-cells and other immune components, leading to inflammation in the skin, joints, and entheses (the connective tissue between tendons or ligaments and bone). The immune response is often abnormally activated by self-antigens, driving the autoimmune process.
- Environmental Triggers: Infections, physical trauma (Koebner phenomenon), and lifestyle factors like smoking and obesity can act as triggers. These factors may alter immune system function, precipitating or exacerbating symptoms in genetically predisposed individuals.
Symptoms to Watch For

While all conditions progress over time, you can keep an eye out for the following symptoms to know when to seek expert intervention:
- Joint Pain and Stiffness: Commonly affects fingers, toes, knees, and lower back. Symptoms may worsen after periods of inactivity.
- Skin Changes: Individuals with psoriatic arthritis often experience psoriasis symptoms, such as red, scaly patches on the skin.
- Swelling: Inflammation can cause fingers and toes to swell, giving them a sausage-like appearance (dactylitis).
- Fatigue: Chronic inflammation can lead to persistent fatigue and reduced energy levels.
- Eye Problems: Conditions like uveitis (eye inflammation) are common among those with psoriatic arthritis, leading to redness and pain.
Advanced Symptoms and Complications

While the common symptoms of joint pain, stiffness, and swelling are well-known, advanced cases of PsA may present with more complex manifestations:
- Enthesitis: Inflammation at the sites where tendons or ligaments insert into the bone (common at the Achilles tendon or plantar fascia) can cause significant pain and mobility issues.
- Spondylitis: PsA can involve the spine, leading to back pain and stiffness. This can sometimes be difficult to distinguish from ankylosing spondylitis, particularly in patients with axial involvement.
- Nail Changes: Up to 80% of PsA patients experience nail changes such as pitting, onycholysis (separation of the nail from the nail bed), or hyperkeratosis. These nail abnormalities can correlate with disease severity.
- Systemic Complications: PsA is associated with an increased risk of cardiovascular disease, metabolic syndrome, and depression. Chronic inflammation can contribute to endothelial dysfunction and increased cardiovascular risk.
- Psoriatic Uveitis: An inflammation of the eye that can cause pain, redness, and blurred vision, requiring prompt treatment to prevent vision loss.
Treatment Approaches
Treatment is tailored to the individual and may include:
- Medications: NSAIDs for pain and inflammation, DMARDs like methotrexate to slow disease progression, and biologics to target specific parts of the immune system.
- Physical Therapy: Helps maintain joint function and mobility.
- Lifestyle Modifications: Regular exercise, maintaining a healthy weight, and avoiding triggers like stress and smoking can help manage symptoms.
Monitoring and Managing Long-Term Complications

Patients with PsA require ongoing monitoring to manage disease progression and associated complications:
- Regular Assessments: Joint counts, patient-reported outcomes, and imaging are used to track disease activity. Tools like the Psoriatic Arthritis Disease Activity Score (PASDAS) or the Disease Activity in Psoriatic Arthritis (DAPSA) can guide treatment adjustments.
- Cardiovascular Risk Management: Regular screening for hypertension, dyslipidemia, and diabetes is recommended. Lifestyle interventions and medications may be required to manage these comorbid conditions.
- Psychosocial Support: Living with a chronic condition like PsA can impact mental health. Access to mental health professionals and support groups can help address issues like depression, anxiety, and social isolation.
The Future of Psoriatic Arthritis Management

Research is rapidly advancing in the field of PsA, with ongoing studies exploring novel therapeutic targets and personalized medicine approaches:
- Precision Medicine: Efforts to understand the genetic and molecular underpinnings of PsA are paving the way for more targeted therapies. Biomarkers predictive of treatment response could help tailor therapy choices to individual patients.
- New Therapeutics: Drugs targeting novel pathways such as IL-23, TYK2, and other inflammatory mediators are under investigation. These agents offer hope for patients who do not respond adequately to existing treatments.
- Patient-Centered Care Models: Integrating rheumatology, dermatology, and primary care can improve overall management, ensuring that skin, joint, and systemic manifestations are all adequately addressed.
What to Remember

Psoriatic arthritis is a multifaceted disease that requires a nuanced, multi-disciplinary approach to management. Early diagnosis, personalized treatment strategies, and comprehensive care can significantly improve outcomes and quality of life for those affected. As research continues to uncover new insights into the disease, patients and clinicians alike can look forward to more effective and tailored approaches to managing this challenging condition.